Peer Reviewed
Infectious Mononucleosis
AFFILIATIONS:
1University of Calgary
CITATION:
Leung AKC, Pinto-Rojas A. An Intriguing Diagnosis: Infectious Mononucleosis. Consultant. Published online: October 13, 2022. doi:10.25270/con.2022.10.000005
DISCLAIMER:
The authors report no relevant disclaimers.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Alexander K. C. Leung, MD, #200, 233 16th Ave NW, Calgary, AB T2M 0H5, Canada (aleung@ucalgary.ca)
An 18-year-old man presented with a 3-day history of fever, sore throat, and neck swelling. His past health was unremarkable, and his immunizations were up to date. There was no history of travel outside the country or of an animal bite or scratch.
The patient's temperature was 39.5°C (103.1°F); pulse, 98 beats/min; blood pressure, 120/80 mm Hg; and respiratory rate, 20 breaths/min. The pharymx and tonsils were erythematous. Whitish exudates were seen in the tonsillar areas (Figure 1). There was an enlarged tender lymph node measuring 3 x 4 cm in the right posterior aspect of the neck (Figure 2). In addition, there were shotty lymph nodes in both cervical areas. There was no lymphadenopathy elsewhere. The spleen and liver were not palpable. A throat swab was taken that proved negative for group A B-hemolytic streptococcus. The patient was treated with benzydamine hydrochloride oral rinse and acetaminophen.

Figure 1. Whitish exudates are seen here in the tonsillar area of an 18-year-old man with infectious mononucleosis.
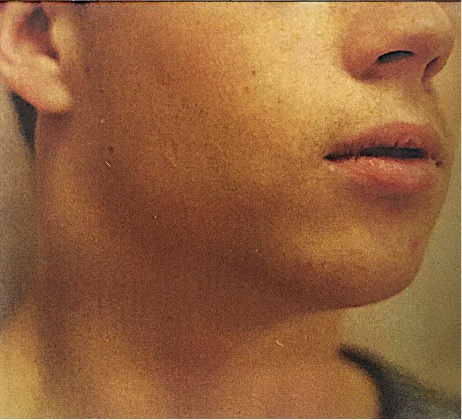
Figure 2. The patient presented with an enlarged, tender lymph node measuring 3 x 4 cm in the right posterior aspect of the neck.
The patient returned 24 hours later with a maculopapular rash covering the whole body (Figure 3). A complete blood count showed a hemoglobin of 12.0 g/dL, a white blood cell count of 1,350/mL with 78% lymphocytes, 15% neutrophils, and 7% monocytes, and a platelet count of 150,000/mL. A monospot test was positive. A diagnosis of infections mononucleosis was made. The patient was seen 3 days later for follow-up. At that time, the rash had started to fade, and the spleen was palpable 2 cm below the costal margin (Figure 4).

Figure 3. Twenty- four hours after the initial office visit, the patient returned with a maculopapular rash covering his entire body.
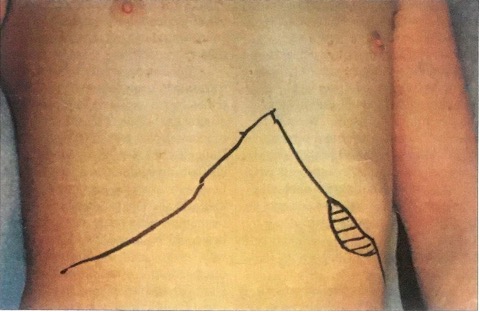
Figure 4. Three days later, the patient's rash had started to fade, and the spleen was palpable 2 cm below the costal margin.
Etiology And epidemiology
Infectious mononucleosis is caused by the Epstein-Barr virus (EBV). It is transmitted primarily in saliva (hence its colloquial appellation, "the kissing disease") and, less commonly, by blood transfusion.
The disease most commonly affects young adults aged 15 to 35 years, with a peak at 15 to 19 years. Early childhood infection is common in persons from low socioeconomic groups. Although primary EBV infection in infancy is almost always asymptomatic, up to 50% of primary EBV infections in adolescents manifest as infectious mononucleosis.
Pathophysiology
The usual outcome of B-lymphocyte infection with EBV is persistent latent infection. EBV infects B cells binding to the cell surface protein CD21, the EBV receptor in B lymphocytes. EBY-infected B lymphocytes trigger T-cell response, which attempts to control the proliferation of infected B cells. A higher concentration of EBV, which probably occurs in adolescents, increases the number of infected B cells. This magnifies the T-cell response and causes symptomatic infectious mononucleosis.
The disease course is associated with the presence of atypical lymphocytes in peripheral blood and internal lymphoid organs. The atypical lymphocytes seen in infectious mononucleosis are T lymphocytes of the CD8+ subset, with a smaller contribution from CD4+ cells. The relative, as well as absolute, increase in CD8+ lymphocytes results in a transient reversal of the normal 2:1 CD4+/CD8+ (helper/suppressor) T-lymphocyte ratio.
Clinical manifestations
The incubation period from the time of viral exposure to development of infectious mononucleosis is approximately 4 to 7 weeks. In children, the incubation period may be shorter. Prodromal symptoms, which may last for 1 to 2 weeks, include malaise, fatigue, headache, arthralgia, and myalgia.
The classic symptoms of infectious mononucleosis are fever, sore throat, and lymphadenopathy. The patient's temperature may reach 38.9°C to 40°C (102°F to 104°F) and may last for 1 to 2 weeks. The pharynx is usually diffusely inflamed. There is often marked tonsillar enlargement with thick tonsillar exudates. Palatal petechiae may be present Lymphadenopathy occurs most commonly in the anterior and posterior cervical lymph nodes but generalized lymphadenopathy may be observed. Splenomegaly is usual, and hepatomegaly may be present. The rash is usually maculopapular and occurs in approximately 10% to 15% of cases. Between 80% and 90% of patients who are treated with antibiotics containing ampicillin or amoxicillin experience a pruritic maculopapular rash.
Laboratory findings
Peripheral blood leukocytosis (10 to 20 x [10.sup.3]/mL) is observed in most patients; lymphocytes make up at least 50% of the white blood cell differential count. Atypical lymphocytes (also called Downey cells) are mature T lymphocytes that have been antigenically activated; they constitute more than 10% of the total leukocyte count. These atypical lymphocytes vary in size but tend to be larger overall and to have vacuolated basophilic cytoplasm; eccentrically placed, indented, or folded nuclei; and an increased cytoplasmic/nuclear ratio (Figure 5).

Figure 5. Aypical lymphocytes constitute more than 10% of the total leukocyte count in infectious mononucleosis. They have vacuolated basophilic cytoplasm; eccentrically placed, indented or folded nuclei; and an increased cytoplasmic/nuclear ratio.
The classic test for infectious mononucleosis is the demonstration of heterophil antibodies. The heterophil antibodies of infectious mononucleosis, also known as Paul-Bunnell antibodies, are IgM antibodies that can agglutinate sheep and horse erythrocytes but not guinea pig kidney cells. This adsorption property distinguishes this response from the heterophil response found in patients with serum sickness and rheumatic diseases and in some normal persons. Quantitative testing by the traditional Paul-Bunnell technique is rarely performed other than in a research setting.
A rapid slide (monospot) test--a qualitative test using the latex agglutination technique--is the most widely used method to detect the serum heterophil antibodies of infectious mononucleosis. The test is unreliable in children younger than 4 years because of the incidence of false-negative results. When confirmation of the diagnosis is required in children younger than 4 years, serologic testing for antibodies to EBV is recommended.
Sequelae
Complications are rare but may include autoimmune hemolytic anemia, aplastic anemia, prolonged hypogammaglobulinemia, thrombocytopenia, splenic rupture, hepatitis, cranial nerve palsy, encephalitis, upper airway obstruction, Guillain-Barre syndrome, "Alice-in-Wonderland" syndrome (distortion of sizes, shapes, and spatial relations of objects), Reye syndrome, myocarditis, and transient arrhythmias. Children with X-linked lymphoproliferative syndrome usually develop fatal infectious mononucleosis. EBV has been shown to have a remarkably strong association with at least five types of malignancies.
Management And prognosis
Treatment is mainly supportive. Reduction of activity and bed rest as tolerated are recommended. Advise patients to avoid contact sports or strenuous exercise for 2 to 3 weeks or while splenomegaly is still present.
Most patients have an uneventful recovery. Children usually recover more quickly than adults.
Dr. Leung is clinical associate professor of pediatrics at the University of Calgary of and pediatric consultant at the Alberta Children's Hospital in Calgary, Alberta. Dr. Pinto-Rojas is associate professor of pathology and laboratory medicine at the University of Calgary.


