Role of Beta-Cell Function in Diabetes
Saturday, October 19 at 4:20 pm and 5:15 pm
LAS VEGAS—Beta-cell function declines over the course of type 2 diabetes and patients may eventually require insulin therapy to achieve or maintain glycemic control. Kevin A. Peterson, MD, MPH, will present data on the importance of maintaining beta-cell function in diabetes patients at this afternoon’s workshop titled, “Applying Beta-Cell Preservation Theory to Everyday Practice.”
Peterson, professor and director of research in family medicine and community health at the University of Minnesota Medical School, will open the workshop with a review of beta-cell physiology and biologic factors influencing beta-cell function. He will also describe recent data demonstrating a correlation between decreasing beta-cell function and the onset and progression of type 2 diabetes.
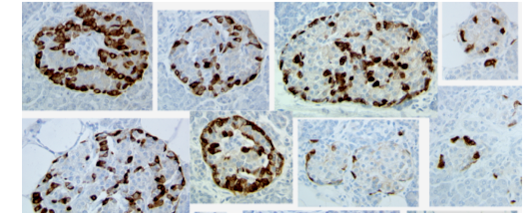
Although no current medication has been demonstrated to clinically regenerate beta-cell function in humans, glucagon-like peptide-1 (GLP-1) receptor agonists have been shown to provide long-term sustainability of control and may be associated with improvement of beta-cell function. FDA-approved GLP-1 agonists include exenatide and liraglutide.
Peterson will highlight the results of a study on exenatide that found after 3 years of treatment with the drug therapy, patients sustained improvements in both acute phase insulin secretion and disposition for at least 4 weeks following cessation of therapy. Liraglutide increases human beta-cell replication in vitro. Clinical trials are ongoing to evaluate beta-cell mass with liraglutide.
Improvement in beta-cell function is not enough to sustain glycemic control, according to Peterson. He will discuss recent STRRIDE (Studies of a Targeted Risk Reduction Intervention through Defined Exercise) and Finnish Diabetes Prevention Study results that suggest moderate activity is the most effective current modality for maintaining beta-cell function.
Peterson will also describe therapeutic strategies leading to beta-cell preservation in patients at risk of developing diabetes. For example, lifestyle intervention is related to the improvement of insulin sensitivity, secretion, and weight loss.
- Eileen Koutnik-Fotopoulos


