Bronchocele
 Left-sided chest pain of less than 24 hours’ duration caused a 39-year-old man to present to the emergency department.
Left-sided chest pain of less than 24 hours’ duration caused a 39-year-old man to present to the emergency department.
He described the pain as non-radiating, sharp, and intermittent, lasting less than 1 minute. The patient had associated shortness of breath with shallow and deep inspirations. He denied any other constitutional symptoms, such as nausea, dizziness, or diaphoresis.
The patient had a 31 pack-year history of tobacco use. Four years earlier, he had been hospitalized for spontaneous pneumothorax that required chest tube placement.
During this hospitalization, he was noted to have a left upper lobe (LUL) pneumonia and underwent bronchoscopy with transbronchial biopsies. The patient was subsequently told that the pathology results were negative for malignancy.
His maternal family history was significant for a LUL mass requiring lobectomy. On a review of systems, he reported a 6-month history of fatigue with associated neck and back pain. On physical examination, it was noted that breath sounds were diminished in the LUL.
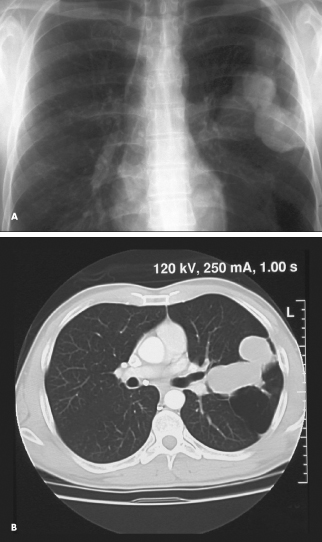
Laboratory results were normal. A chest radiograph showed a lobulated mass extending into the left hilar region (A). A CT scan of the thorax revealed a lobulated low-attenuation branching mass in the LUL secondary to chronic bronchial obstruction (B).
The clinical presentation was consistent with a bronchocele. The patient was scheduled to follow-up for an outpatient evaluation for thoracoscopic biopsy. Unfortunately,
he did not keep this appointment and has been unavailable for further work-up.
Bronchoceles may be caused by abnormal or excessive mucus production, which may occur in cystic fibrosis or bronchial asthma. They may result from segmental or subsegmental bronchial occlusion caused by congenital atresia or inflammatory stricture. In rare instances, a bronchial neoplasm may be the underlying cause. The bronchocele in this patient was probably secondary to congenital atresia.


