12-year-old girl with bullous rash
 HISTORY
HISTORY
A 12-year-old girl had fever, headache, nausea, and a papular and bullous rash of 4 days’ duration. The rash initially appeared on the dorsal surfaces of the hands and feet and spread centrally to involve most of her body surface.
Three weeks earlier, she presented with multiple small abscesses on her abdomen and was treated with a 10-day course of trimethoprim/sulfamethoxazole (TMP/SMX) for methicillin-resistant Staphylococcus aureus infection. This was her first exposure to TMP/SMX or any sulfa-containing medication. She had no known allergies.
PHYSICAL EXAMINATION
Temperature, 38.8ºC (101.8ºF); heart rate, 105 beats per minute; blood pressure, 90/53 mm Hg. Child had marked periorbital and bilateral upper extremity edema and numerous tense vesicles and bullae (ranging from a few millimeters to 3 cm) interspersed with dusky papules on the trunk, arms, legs, face, and scalp. Palms, soles, conjunctivae, mucous membranes, and vaginal mucosa were spared. Nikolsky sign was negative. No significant lymphadenopathy was present.

LABORATORY FINDINGS
White blood cell count, 18,100/µL, with 18% bands and 12% atypical lymphocytes. Aspartate aminotrans-ferase, 78 U/L; alanine aminotransferase, 117 U/L; g-glutamyltransferase, 314 U/L; bilirubin, 4.2 mg/dL (total) and 2.2 mg/dL (direct); C-reactive protein, 3.2 mg/L. Results of urinalysis, urine culture, and monospot screen were normal.
Results of tests for antinuclear antibody, C3 and C4, quantitative IgG and IgM, cytomegalovirus (CMV) IgG and IgM, hepatitis (A, B, and C) and Epstein-Barr virus (EBV) serologies, adenovirus IgG and IgM, and culture of bullous fluid and mucous membranes for herpes simplex virus were all negative.
WHAT’S YOUR DIAGNOSIS?

 Cutaneous drug reactions represent a wide spectrum of clinical presentations that result from hypersensitivity to a medication. Drug reaction with eosinophilia and systemic symptoms (DRESS) is a rare, severe reaction, reported to result from a variety of medications, most often from aromatic anticonvulsants and less frequently from sulfonamides. Other drugs, including allopurinol, minocycline, calcium channel blockers, and ranitidine, have been implicated.1-5 About 2% to 3% of all hospitalized patients experience adverse cutaneous drug reactions.1,6 Prompt and accurate diagnosis is essential; the complications of DRESS may be severe, and treatment beyond simple discontinuation of the offending medication is often required.
Cutaneous drug reactions represent a wide spectrum of clinical presentations that result from hypersensitivity to a medication. Drug reaction with eosinophilia and systemic symptoms (DRESS) is a rare, severe reaction, reported to result from a variety of medications, most often from aromatic anticonvulsants and less frequently from sulfonamides. Other drugs, including allopurinol, minocycline, calcium channel blockers, and ranitidine, have been implicated.1-5 About 2% to 3% of all hospitalized patients experience adverse cutaneous drug reactions.1,6 Prompt and accurate diagnosis is essential; the complications of DRESS may be severe, and treatment beyond simple discontinuation of the offending medication is often required.
PATHOPHYSIOLOGY
Predisposition to hypersensitivity reactions to sulfonamides is suspected to be related to polymorphisms in N-acetyl transferase, an enzyme involved in a major metabolic pathway for sulfonamides.7 Patients with a slow acetylation phenotype produce a larger amount of reactive intermediates, because they have an inherited reduction in their capacity to detoxify such metabolites. Hydroxylamine and nitroso metabolites are thought to be responsible for toxicity, with tissue injury
occurring via an immune-mediated reaction.7,8
CLINICAL MANIFESTATIONS
DRESS typically occurs 1 to 8 weeks after first exposure to an offending agent. It begins with fever followed by a cutaneous eruption and variable internal organ involvement.1,6,9 The affected organs, in order of frequency, include the skin, liver, kidneys, lungs, and heart; rarely, the CNS, thyroid, pancreas, GI tract, and muscles are involved. Multivisceral involvement in DRESS is what differentiates it from more common cutaneous drug reactions.1,7-10
DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS
Given its variable presentation, DRESS can be difficult to diagnose. Although a definitive definition of DRESS is lacking, diagnostic criteria have been proposed by Kardaun and colleagues.4 Following these criteria, our patient’s presentation was consistent with DRESS (Table 1). Eosinophilia was noted on day 4 of admission. Although results of all viral serologies were negative in this patient, an association between either primary viral infection or reactivation of a virus (such as human herpesvirus 6, CMV, and EBV) and the development of this hypersensitivity reaction has been reported by multiple studies.11,12 Whether the presence of the infection is a prerequisite for the development of DRESS, or whether DRESS predisposes to the development or reactivation of these infections, has yet to be elucidated.
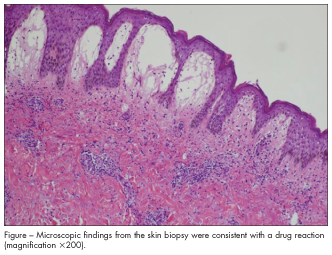
The differential diagnosis of DRESS includes other dermatoses, infectious processes, and autoimmune disorders (Table 2), which may be indistinguishable without pathologic evaluation of a biopsy of the affected skin.1,10 In this patient, skin biopsy revealed prominent spongiotic dermatitis and subepidermal blisters with severe papillary edema as well as superficial and focally deep perivascular inflammatory cell infiltrate composed of lymphocytes, macrophages, eosinophils, and rare neutrophils, consistent with a drug reaction (Figure).

 TREATMENT AND PREVENTION
TREATMENT AND PREVENTION
DRESS is a potentially life-threatening clinical entity that requires prompt treatment. This involves immediate withdrawal of the offending agent and supportive care. Other management options remain controversial. Several independent case studies have demonstrated dramatic clinical and laboratory improvements after initiation of systemic corticosteroids. The therapeutic role of systemic corticosteroids in DRESS seems to be supported by the fact that relapses have occurred after rapid tapering or withdrawal of this treatment. The mechanism of benefit may be related to a reduction in eosinophil accumulationeosinophil infiltration is currently thought to contribute to internal organ injury. However, the efficacy of systemic corticosteroids in DRESS has not been substantiated by randomized controlled trials, and they must be used with vigilance.1,6,13,14
Patients who have had a reaction consistent with DRESS should avoid use of similar agents in the future; reexposure to the same drug may result in reappearance of severe symptoms as early as one day after rechallenge.1,14 Susceptible persons may be genetically predisposed to the development of DRESS because of variations in their ability to metabolize the causative compounds. Thus, first-degree relatives of patients who have had a severe hypersensitivity reaction should be counseled about the risk of such reactions to similar drugs. Familial cases have been reported.
COMPLICATIONS
Hepatitis, interstitial nephritis, renal failure, pneumonitis, cardiac and neural toxicity, and severe hematologic abnormalities may develop days to weeks after
the cutaneous manifestations. Hypothyroidism may occur 1 or more months after the initial exposure and may persist up to 2 years.
PATIENT OUTCOME
When DRESS was considered to be the most likely diagnosis, the child was admitted, and treatment with methylprednisolone, 2 mg/kg IV every 12 hours, was started. A dramatic response to therapy was noted on day 4 of hospitalization; she had a marked decrease in edema, erythema, and pain, and laboratory values had begun to normalize. She was discharged home on hospital day 6 to complete a 6-week tapering course of prednisone. At follow-up, she had no organ-specific injuries, and her skin had healed without scarring.
1. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996;15:250-257.
2. Crowell CS, Melin-Aldana H, Tan TQ. Fever, rash, and hepatic dysfunction in a 3-year-old child: a case report. Clin Pediatr (Phila). 2008;47:517-520.
3. Garnier A, El Marabet el H, Kwon T, et al. Acute renal failure in a 3-year-old child as part of the drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome following hepatitis A. Pediatr Nephrol. 2008;23:667-669.
4. Kardaun SH, Sidoroff A, Valeyrie-Allanore L, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609-611.
5. Lee AY. Fixed drug eruptions: incidence, recognition, and avoidance. Am J Clin Dermatol. 2000;1:277-285.
6. Mockenhaupt M. Severe drug-induced skin reactions: clinical pattern, diagnostics and therapy. J Dtsch Dermatol Ges. 2009;7:142-162.
7. Rieder MJ, Uetrecht J, Shear NH, Spielberg SP. Synthesis and in vitro toxicity of hydroxylamine metabolites of sulfonamides. J Pharmacol Exp Ther. 1988;244:
724-728.
8. Sullivan JR, Shear NH. The drug hypersensitivity syndrome: what is the pathogenesis? Arch Dermatol. 2001;137:357-364.
9. Pickert CB, Belsha CW, Kearns GL. Multi-organ disease secondary to sulfon-amide toxicity. Pediatrics. 1994;94:237-239.
10. Bachot N, Roujeau JC. Differential diagnosis of severe cutaneous drug eruptions. Am J Clin Dermatol. 2003;4:561-572.
11. Descamps V, Valance A, Edlinger C, et al. Association of human herpesvirus 6 infection with drug reaction with eosinophilia and systemic symptoms. Arch
Dermatol. 2001;137:301-304.
12. Seishima M, Yamanaka S, Fujisawa T, et al. Reactivation of human herpes-virus (HHV) family members other than HHV-6 in drug-induced hypersensitivity syndrome. Br J Dermatol. 2006;155:344-349.
13. Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update. Dermatology. 2003;206:353-356.
14. Wolf R, Orion E, Marcos B, Matz H. Life-threatening acute adverse cutaneous drug reactions. Clin Dermatol. 2005;23:171-181.


